Tummy pain is one of the most common children’s health complaints, ranging from a quick 24-hour bug to persistent, daily aches for months on end. Chronic digestive pain can be debilitating, interfering with school, sports, friendships, and an overall balanced lifestyle. A chronically upset stomach can be caused by a range of factors such as infection, stress and anxiety, an imbalanced microbiome, and, less commonly, inflammatory diseases like Crohn’s and ulcerative colitis. These last two conditions are genetically driven autoimmune disorders, known as Irritable Bowel Disorders (IBD), and are important to rule out when there is chronic digestive discomfort. More concerning symptoms include bleeding, lack of appetite, and severe, chronic pain, which warrant a checkup with your family doctor for further evaluation.
When more concerning causes are ruled out, often the cause of chronic digestive complaints is diagnosed as irritable bowel syndrome (IBS). IBS is linked to imbalance in the microbiome due to various factors such as a round of antibiotics that knocked back beneficial bugs, acute viral infection, poor quality nutrition, or chronic anxiety that impacts gut motility and acidity.
Bathroom Scale
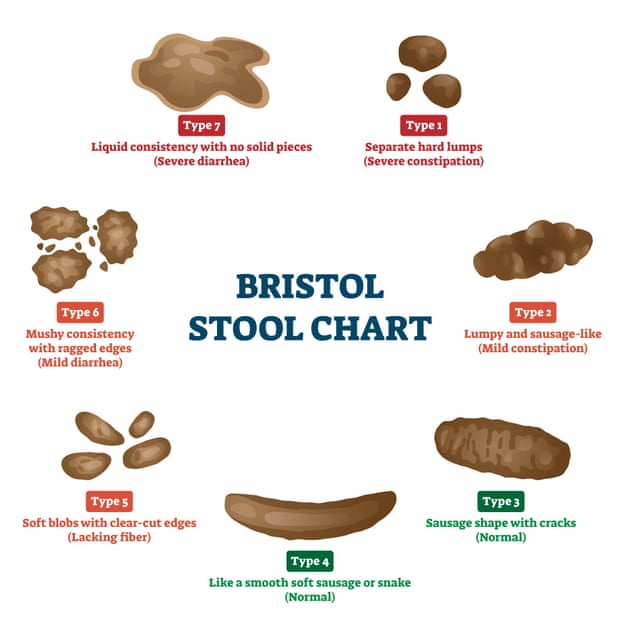
There are a few telltale symptoms that point to an IBS diagnosis. One of the best ways to determine what’s going on is to check out the toilet bowl to assess the shape and consistency of stool. We doctors are always interested in bowel movements because they provide insight into the inner workings of the digestive system, aiding in making a correct diagnosis. The best resource available is the Bristol Stool Chart (or Scale), developed at the British Royal Infirmary in Bristol, England in 1997. A quick online search will pull up a visual Bristol Scale for home use and depicts different types of stools ranged by type from 1 to 7, starting with constipation and moving to diarrhea. If your child’s stool looks lumpy and dry, this is a sign of constipation, and if they trend more towards smooth, snake-like shapes, separate blobs, or liquid, this points to diarrhea. An ideal stool is firm, sausage-shaped, brown, and should sink in the toilet.
The Rome III criteria for functional digestive disorders is another commonly used diagnostic assessment, developed by a symposium of gastroenterologists to help doctors confidently diagnose IBS and avoid missing more concerning disease like the IBDs mentioned above. Rome III criteria require the patient to have chronic digestive discomfort for three days per month over the prior three-month period, with symptoms starting at least six months prior.
The child’s symptoms also need to match the following three points:
- Pain symptoms are lessened with a bowel movement
- Symptom onset is related to a change in stool frequency
- Symptom onset is related to a change in stool appearance
If your child meets the above criteria, your family physician will often give an IBS diagnosis without further testing if there are no other signs or symptoms of severe inflammatory disease. After a diagnosis, an effective treatment approach will focus on supporting your child’s microbiome.
Microbiome Balancing Act
The amazing microbiome is key to physical, mental, and emotional wellness. Gut bugs help us digest key nutrients, synthesize neurotransmitters for brain function, keep our immune system strong, and balance inflammation. IBS is a clue that something’s not quite right with microbial balance, involving an overgrowth of an opportunistic bacteria or yeast and a decline in healthy flora. The fibre-rich nutrition from whole fruits, veggies, and whole grains provides complex starches that feed beneficial bacteria. All types of berries, as well as tubers like yams and sweet potatoes, are especially good for the microbiome, providing rich, prebiotic fibre. Cultured foods like unsweetened yogurt, sauerkraut, and apple cider vinegar contain helpful strains like Lactobacillus bulgaricus and Streptococcus thermophilus. Avoiding sugar, juice, fried foods, and chemicals and preservatives in the diet goes a long way as well. Food allergies and sensitivities are another potential cause of underlying inflammation leading to IBS-related symptoms, and your doctor can help with either testing or an elimination challenge protocol to uncover potential triggers. Last, checking in with stress level is critical. Chronic childhood anxiety is strongly linked with digestive imbalance, and vice versa. Once nutritional and lifestyle factors have been addressed, there are tried and true herbal remedies for childhood IBS.
Herbal Tummy Tamers
There are a number of helpful herbals for children’s digestive support, and we’ll focus in on three that are particularly beneficial.
Peppermint
Peppermint has a long history of use as a folk remedy for tummy troubles, often taken as a tea, which is a great place to start particularly for younger children who can’t swallow capsules. For older children with IBS, GI-friendly peppermint oil capsules are one of the most promising treatment options available, with quite a bit of supporting evidence to back it up. Not only does peppermint has antimicrobial properties and decreases nausea, it also acts as a soothing relaxant, or carminative herbal medicine, helping calm smooth muscle spasms in the digestive system. A placebo-controlled 2013 study in The Journal of Pediatrics found that peppermint oil capsules reduced IBS-related pain in 75 percent of children receiving treatment. A 2005 study in India found peppermint oil caps especially effective for diarrhea-type IBS, improving pain and stool consistency with regular use. With peppermint oil, purchasing a quality, enteric-coated capsule is important. Do not swallow peppermint oil directly, as it will burn the esophagus and mucus membranes if not delivered correctly.
Fennel
Fennel is a hardy, perennial herb with feathery leaves that has a distinctive, black licorice flavour and a long history of traditional medicinal use for stomach upset in the Mediterranean region. Like peppermint, fennel oil relaxes smooth muscle spasms to ease pain and discomfort. A 2016 research trial in Italy found fennel oil vastly improved IBS symptoms and quality of life in one month, relieving abdominal pain and bloating, improving stool consistency, and decreasing trips to the bathroom. You may also find peppermint oil combined with fennel oil extract in supplements as both have strong safety profiles when taken correctly: on an empty stomach with a full glass of water.
Papaya
Papaya has traditionally been used in Latin America for digestive discomfort, often taken as whole fruit or juice, and is known for its ability to break down food and reduce inflammation. Papain is a proteolytic enzyme found in papaya fruit that digests proteins into smaller peptides and amino acids, making them easier to digest. Recent research conducted by the International Scientific Group of Preventative Medicine in Vienna discovered that papain reduced constipation, bloating, and painful bowel movements in patients with IBS during a placebo-controlled trial. The authors suggest that papaya enzyme extracts both relieve IBS symptoms and can be used to support healthy digestive tract physiology.
Alongside lifestyle and nutritional changes, administering a combination of peppermint, fennel, and papaya is a safe, effective, and research-supported approach to childhood IBS. For children suffering from this frustrating condition, improving digestive health has a positive impact on their overall quality of life by reducing pain, discomfort, and bathroom trips, helping them get back to the things they love.
You may also enjoy: Simple Ways to Improve Your Child's Gut Health After Antibiotics, The Signs, Causes, and Impact of Constipation in Kids, and Natural Remedies for Child Constipation.









